Diabetic Retinopathy
Diabetic Retinopathy and its causes
Introduction:
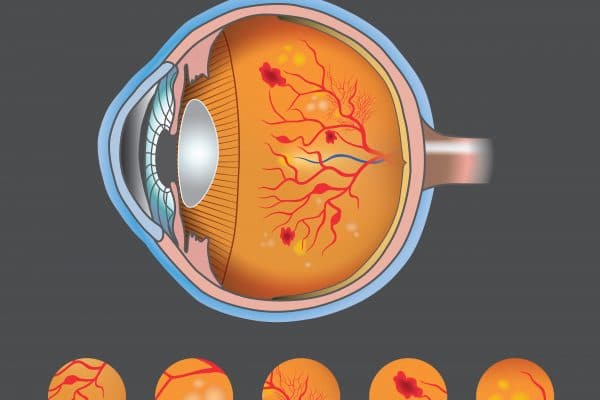
The retina is the deepest layer of the eye, and includes more than 120 million photoreceptor cells, as it captures light and converts it into nerve impulses that travel to the brain through your optic nerve, giving you the ability to see.
The retina is part of the nervous system, the retinal cells do not regenerate and does not multiply like the case with the cells of the nervous system. Therefore, any disease affecting the retina in the eye must be treated as soon as possible to avoid damage to the retina and then the permanent loss of its function.
The basic cause of diabetes varies depending on the type, but regardless of the type of diabetes you have, it can lead to increase of blood sugar.
Sugar retinopathy is one of the complications of diabetes that affects the eye. The longer the duration of diabetes and the lower the control on the blood sugar level, the greater the possibility of complications in the eye.
This disease occurs due to damage of the nutritional blood vessels to the retina tissues sensitive to light in the back of the eye.
Diabetic retinopathy often affects both eyes.
Initially, the diabetes retinopathy may not result in any symptoms or may cause just minor vision problems, in the end it can cause blindness.
Diabetic retinopathy symptoms:
The sense of sight is not clearly affected unless the diabetic retinopathy has advanced, and it may not be accompanied by any pain or symptoms in the early stages of the disease, so it is preferable to perform the detection of eye disorders associated with diabetes on an annual basis to detect the initial signs of symptoms through eye images.
As the condition worsens, symptoms of diabetic retinopathy may include:
- Dark patches or strings floating in the vision often described as spider webs.
- Blurred vision.
- Fluctuating vision.
- Poor color vision.
- Sudden and complete loss of vision.
What are the complications of diabetic Retinopathy?
Diabetic retinopathy includes abnormal growth of blood vessels in the retina. Complications can lead to serious visual problems:
- Vitreous hemorrhage
- The retina detachment
- Glaucoma (cataract)
- Blindness
Prevention
Remember that diabetes is not necessary causes loss of sight, because performing an active role in controlling diabetes can contribute greatly to preventing complications.
You can reduce your risk of developing diabetic retinopathy by doing the following:
- Control your diabetes: by making healthy food and physical activity part of your daily routine.
- Monitor your blood sugar level.
- Ask your doctor about a HbA1c test.
- Maintaining blood pressure and keeping cholesterol levels under control.
- If you smoke, ask your doctor for help to quit.
- Watch for changes in your eyesight.
How is diabetic retinopathy treated?
Treatment depends on several factors, such as the patient’s general health, age, accompanying symptoms, and severity of the injury.
- Treatment in the early stages: Doctors may suffice with monitoring the affected eye, and some patients may be required to do a comprehensive eye examination every 2-4 months.
- Treatment in the advanced stages: If the patient suffers from vision changes, he must start treatment immediately
There are three options for treating diabetic retinopathy:
- Laser treatment:
The laser cauterizes the blood sacs that lead to liquids supply to the retinal tissue, bearing in mind that if you have blurred vision as a result of swelling of the central spot before surgery, your normal vision may not be fully regained to its normal condition, but in some cases, vision actually improves.
- Injection treatment:
A drug is injected into the vitreous of the eye, and these drugs may help stop the growth of new blood vessels by blocking the effects of growth signals that the body sends to create new blood vessels.
- Vitrectomy:
This treatment is used when there is bleeding in the eye or when the retina detaches through surgery in which the vitreous gel is pulled out.